Objective: Tracheal injuries are rare and often devastating. Appropriate management depends on meticulous planning and complex support networks. Multidisciplinary management often may include cardiothoracic surgery, plastic surgery, assist device teams, anesthesia, and pulmonary/trauma critical care experts. The objective of this video is to demonstrate several tools and techniques that were used to salvage a traumatic posterior membranous tracheal tear that occurred during an intubation in the field.
Methods: The techniques demonstrated in this video include bilateral mainstem tracheal intubation, intercostal and latissimus muscle flap buttress of the membranous tear, surgical exposure of the entire posterior trachea, extracorporeal membranous oxygenation (ECMO) through an Avalon cannula, bronchoscopy, and ventilator management.
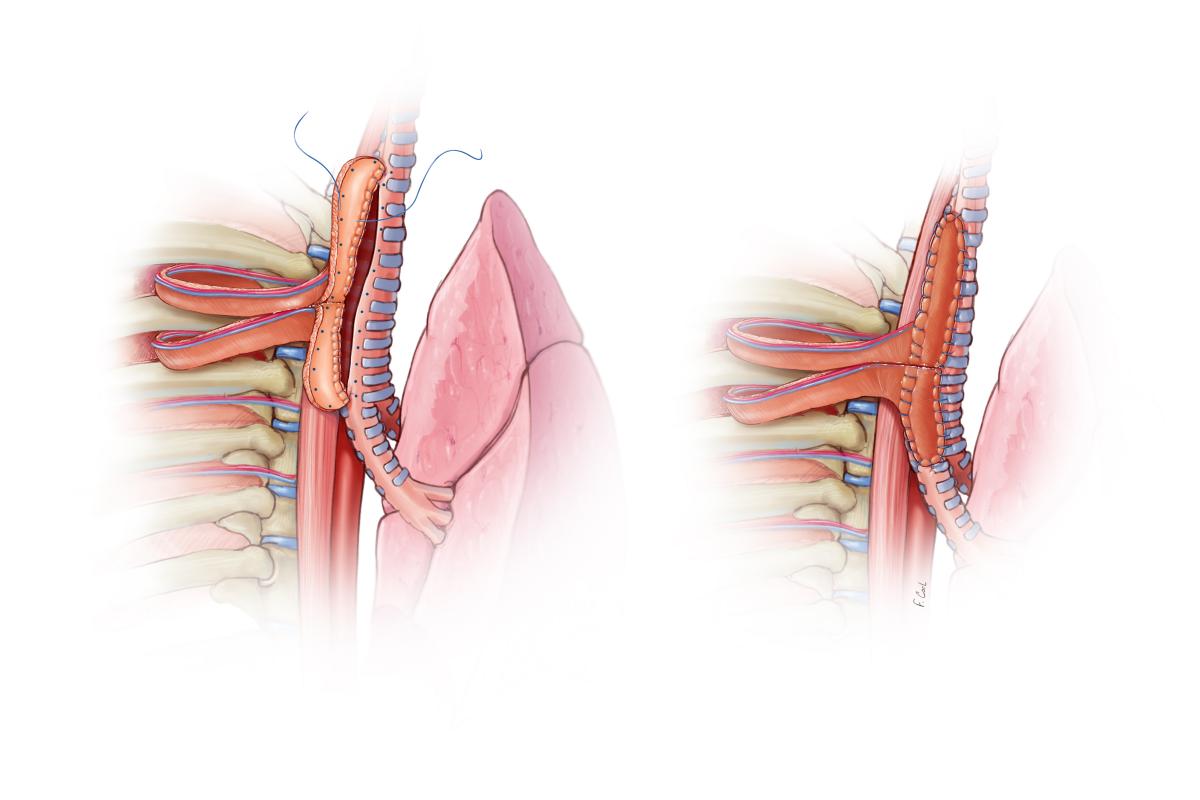
Results: A 48-year-old woman was emergently intubated at her home and developed massive subcutaneous emphysema. A CT scan at an outside facility confirmed that her endotracheal tube had penetrated the membranous posterior trachea at the level of the carina. A bronchoscopy confirmed the injury. Her tube was repositioned and she was transferred for a higher level of care. The patient was taken immediately to the operating room, where she had an emergent tracheostomy with placement of a long, armored size 6.0 endotracheal tube advanced through the tracheostomy and into the left mainstem bronchus. A long, pediatric, 5.0 endotracheal tube was placed into the right mainstem bronchus orally and secured to a molar to prevent extubation. The patient was weaned from the ventilator, placed on broad spectrum antibiotics, and resuscitated. She returned to the operating room 48 hours later. Two intercostal muscle flaps and a latissimus dorsi muscle flap were utilized for the repair through a right 3rd-4th interspace posterolateral thoracotomy. A segment of the 4th rib was removed to create a window through which the latissimus was placed. At the termination of the case, the patient was not able to adequately oxygenate and ventilate herself, therefore veno-venous ECMO was initiated. She was able to be successfully weaned from ECMO and tracheostomy was removed prior to transfer to rehabilitation facility. The patient is now 3 months post-surgery and continues to do well.
Conclusions: Complex management teams working in a multidisciplinary manner can salvage major tracheal injuries.
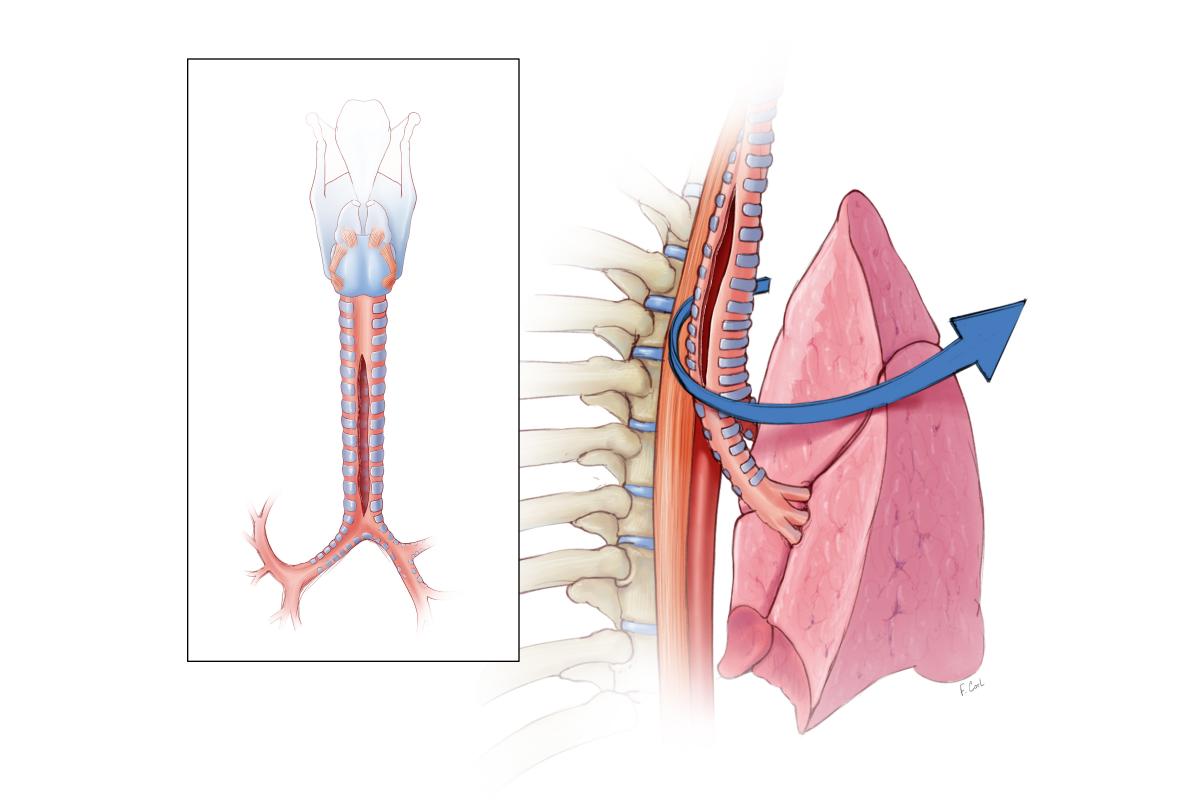
Figure 1: An open tracheostomy was performed and through this a long 6.0 armored endotracheal tube was placed in the left mainstem bronchus. A long, pediatric 5.0 endotracheal tube was placed into the right mainstem bronchus orally.
Figure 2: Surgical approach was via right thoracotomy which provided optimal access to the trachea and both proximal mainstem bronchi.
Figure 3: The repair was performed using two intercostal muscle flaps, inset to recreate the membranous portion of the trachea over a distance of 8 cm.
Additional Authors: Craig Daniels, Richard Patch, and Gregory Schears.



An utterly stunning surgical tour de force and finesse
Also I’d venture a guess that this isn’t the first (albeit maybe the first survivor of) such injury in association with an intubating bougie passed down a main stem followed by an overly deep follow-on thrust with the ETT.
A very good operation.I do not understand the methods of the menbrane reconstruction. Why not direct suture of the membrane, and then covered with muscle flap, could you tell me the details of the reconstruction? For example, which layer of the intercost muscle will be locted inside? sutured tow sides of the tear? In addition, how do you remove the muscles in the trachea after surgery,and when?Thank you very much
Congratulations .
Injury of trachea are challenging .
Did you consider primary repair of the trachea as emergency surgery,follow by tracheostomy ? I understand that she admitted same day after injury, is it right?
Thank you.
Congratulations for your challenging operation. I also experienced a similar case of traumatic posterior membranous tracheal rupture. We repaired the rupture primarily under cardiopulmonary bypass support without using any muscle flaps. Do you think muscle flaps are mandatory for these kinds of injuries?
Thank you very much..